Why Mean Flow is Key to Assessing Graft Patency
 Mean flow, maximum flow, minimum flow, PI, DF% or D/S Ratio all show up on the flow monitor display. What should the surgeon consider first in assessing the patency of a bypass graft?
Mean flow, maximum flow, minimum flow, PI, DF% or D/S Ratio all show up on the flow monitor display. What should the surgeon consider first in assessing the patency of a bypass graft?
Mean flow is the primary indicator of graft patency. It can confirm the patency of a good graft or, conversely, signal an undesirable graft. While flows greater than 20 to 30 mL/min indicate a good graft, flows under 5 mL/min always indicate that there is a problem with the graft. Experience supports a mean flow of 30 mL/min to indicate acceptable patency. For small patients or small target vessels, this number can be reduced to 20 mL/min. European guidelines state: “Flow < 20 mL/min and pulsatility index >5 predict technically inadequate grafts, mandating graft revision before leaving the operating theatre.”1
Flow Indicating a Graft in Trouble
A high mean flow always indicates a viable graft, and near-zero flow always indicates a graft in trouble. Mean flow alerts the surgeon to one of three graft conditions: Mean flow > 20 mL/min, the graft provides adequate flow and may be considered patent; mean flow < 5 mL/min is unacceptably low, the graft is compromised and requires further examination; mean flow between 5 mL/min and 20 mL/min signals a questionable graft that should be analyzed further.
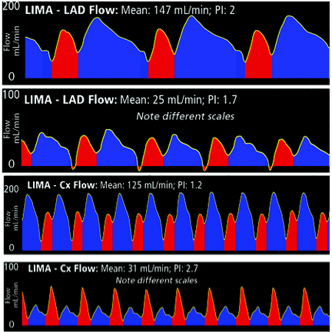
If graft mean flow is still less than expected after flow is measured with the native coronary temporarily occluded to assess competitive flow, the surgeon might consider other factors that influence and possibly limit mean flow. These include kinks, twists in the graft, back wall stitch, thrombus, low mean arterial pressure, vasospasm, small patient, small target vessel, small graft capacity, poor myocardial runoff. But remember: Mean flow is key to successful graft patency assessment.
1The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS), “Guidelines on Myocardial Revascularization,” Eur J Cardiothorac Surg 2010; 38, S1 S52.




