Case Reports Demonstrate the Importance of Measuring Flow

Flow, the amount of fluid passing a certain point during a defined time frame (mL/min, L/min), is life’s quintessential vital sign. By delivering oxygen and nutrients to cells for metabolism and removing metabolic wastes, blood flow is life-giving. When blood fails to flow, life ends.
Whether a CABG is performed minimally-invasively, off-pump, on-pump, or robotically-assisted, the end point is the same: to know how much blood flow is going through a newly created anastomosis. A quantitative flow measurement takes only seconds to perform. The flow measurement augments a surgeon’s clinical observations such as the quality of the heart’s contractions, MAP, EKG, CO, and BP. Direct graft flow measurements help a surgeon identify a problem’s source more effectively and efficiently than any other single parameter as illustrated by the following two CABG cases where revisions were triggered by unacceptable flow measurements.
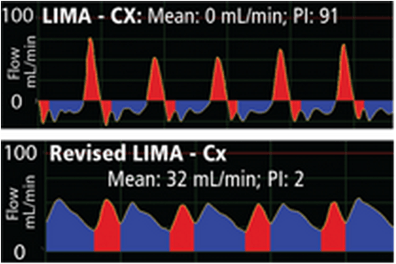
Case #1: A 78-year-old female patient underwent a single coronary bypass grafting to bypass a blocked circumflex (Cx) coronary artery with the left internal mammary artery (LIMA) graft. Following the anastomosis of the LIMA to the Cx, flow was measured with a perivascular Coronary Flowprobe and measured 0 mL/min. The Pulsatility Index (PI) for the bypass graft was 91. Moreover, the flow waveform exhibited a spiky systolic profile which further triggered revision of the graft anastomosis.
Following revision of the graft, the mean flow of the graft improved to 32 mL/min with a PI of 2. The waveform now exhibited a balanced systolic/diastolic profile (bottom waveform) and the patient’s prognosis was good. The first zero mean flow reading was the determining factor in the decision to revise and save the graft.
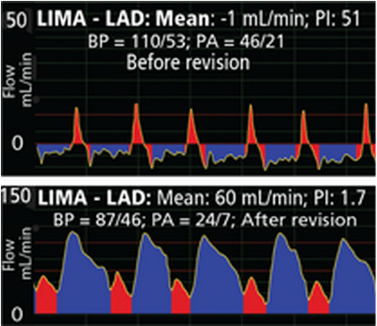
The poor mean flow of the first flow measurement demonstrated a graft that required immediate attention. Mean flow was -1 mL/min. The LIMA to LAD anastomosis was revised and mean flow improved to 60 mL/min with a excellent diastolic dominant flow pattern.
Case #2: An 80-year-old female underwent CABG to bypass a blocked left anterior descending coronary artery (LAD). Her left internal mammary artery (LIMA) was anastomosed to the LAD distal to the blockage. Following the anastomosis, LIMA - LAD flow measured -1 mL/min. The PI was 51. Blood pressure was 110/53 and pulmonary arterial pressure was 46/21. The patient’s deteriorating BP, poor mean flow, high PI and poor waveform profile indicated the immediate need for revision to the graft. Following revision, mean graft flow increased to 60 mL/min, PI improved to 1.7 and the waveform exhibited a classic LIMA-LAD profile with a strong diastolic component. Blood pressure decreased to 87/46 and pulmonary arterial pressure decreased 24/7. The patient’s outcome was good.




