CKD ESKD Life Plan and Access Plan
Preferences come in all shapes and sizes, and in many medical situations, we’re taught to ignore them. However, in some cases, preferences may be the most important medical criterion of all…
I was recently honored to be a faculty member of the National Kidney Foundation of Arizona's 24th Southwest Nephrology meeting: "Change to Advance Kidney Care." I’ve spent my career working to improve ESKD treatment, so my presentation title (to no one’s surprise) was: “The Current State of Vascular Access for the Physician and Nursing/Dialysis Technician.”
The KDOQI 2019 Vascular Access Guidelines were released in the spring of 2020, just as COVID-19 avalanched down onto the medical community, so full implementation is understandably lagging. Consequently, I focused my presentation on three topics:
- Clinical issues related to AV fistula needle design and ways to mitigate patient risk.
- The ESKD Life-Plan and related KDOQI 2019 Guideline implementation based on the Life-Plan concept.
- Specific guidelines related to routine care and cannulation of AV accesses.
The 2019 guidelines use an individualized Life-Plan and supporting Access Plan to meet the needs of an individual with CKD over the course of their lifetime. Treatment modalities can include conservative management, hemodialysis (in-center, home, or nocturnal), peritoneal dialysis (PD), and kidney transplantation…
…But this choice should be based on the individual's preferences in every way that is medically acceptable. This idea seems simple, but is still gaining full traction, so it subtly undergirded much of my presentation.
The Life-Plan (a patient’s personal desires for mobility, activity, specific times with family and friends, etc) guides modality selection, and then the Access Plan is created to support that modality. For example, if PD is the patient’s initial choice, then vessel preservation for AV access should follow the individual’s transition to the second modality. The Access Plan to support the PD would be the insertion of a catheter followed by its care and maintenance. If the PD modality needs to transition to hemodialysis, then the Access Plan shifts to AV access creation, contingency, and succession.
However, the first priority is preservation of vessels that might be needed for future vascular access. This should be an immediate consideration when the CKD risk is first identified. We accomplish preservation by coordinating lab draws and utilizing the hand for IV sites to reduce venipunctures.
So the basic planning process is as follows: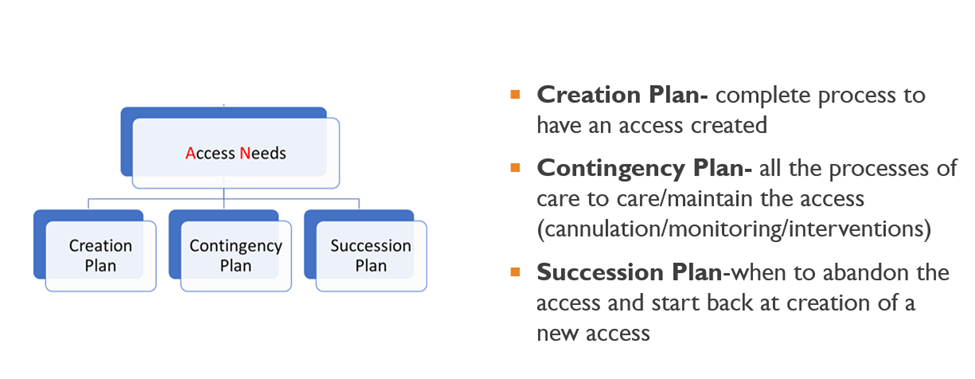
The Contingency Plan must include the routine care and maintenance of the AV access. This includes the choice of cannulation method, monitoring and surveillance of the vascular access, referral for any interventions, and then evaluation of the outcomes. The process of care is continuous until the current vascular access must be abandoned. Then the process begins again with the Creation Plan for the next access.
The Transonic HD03 Monitor is the perfect companion to the process. Our Delivered Flow and Recirculation measurements support the Contingency Plan as part of the ongoing monitoring & surveillance to detect catheter dysfunction. With the addition of our Access Flow measurement, the HD03 becomes an essential part of the monitoring and surveillance for early warning of AV fistula or AV graft dysfunction.
Thanks for reading,
Transonic Systems, Inc
The Measure of Better Results



