Proactive Cardiac Function Monitoring during Hemodialysis
By Susan Eymann, MS05 Nov 2015
“The ability to monitor cardiac output is one of the important cornerstones of hemodynamic assessment ...in particular in patients with pre-existing cardiovascular comorbidities.” 1
It is incumbent upon the nephrologist to order periodic cardiac function tests, and track the results along with its associated vascular access flow rates. While access flow remains fairly constant during a hemodialysis treatment, cardiac output decreases an average of 20% during the treatment causing less blood flow to be available to sustain the body’s vital functions. A healthy body will respond to this by increasing peripheral resistance to sustain the blood supply to the heart and brain. Other considerations include:
- The site of a vascular access affects average flow values. Upper arm sites typically have higher flows than lower arm sites.
- Patients with initial high flow fistulas are at greater risk for cardiovascular problems. A fistula may over-mature and present a flow over 2 L/min.
- Autologous fistulas tend to remain sufficiently patent to sustain dialysis at lower flows than do prosthetic grafts.
- A straight upper arm prosthetic graft may initially exhibit an overly high flow. Graft flow tends to decrease over time, so banding a prosthetic graft is not advised. Access flow and cardiac function of these patients should be monitored monthly to ensure that access flow drops before cardiac complications arise.
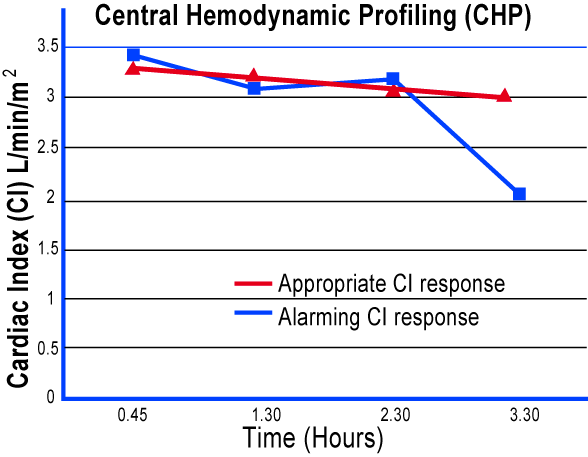
1 Tucker T et al, "Central Hemodynamic Profiling (CHP) during Outpatient Hemodialysis (HD)," J Am Soc