Transonic VA Surveillance Identifies Patients at Risk
“Adequate blood flow in peripheral hemodialysis fistulae and grafts is vital to the success of hemodialysis and to the survival of the patient. Reduction in flow ... presages failure of the access device itself. Access flow can therefore be considered a fundamental property of the access that should be monitored.” Depner TA, MD, UC Davis
Access flow is the quintessential vital sign for an AV Access. Insufficient flow causes underdialysis. Still, lower flow invites thrombosis. Too much flow can lead to heart problems. Each condition harbors associated morbidities. Vascular access surveillance with Transonic Hemodialysis Monitor identifies end-stage renal disease (ESRD) patients at risk for underdialysis, thrombotic events and cardiac failure. 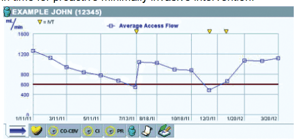
Transonic ultrasound dilution technology is recognized as the “gold standard” intra-access flow measurement technology for hemodialysis patient surveillance during a dialysis session. The method uses Transonic Hemodialysis Monitors and
Flow/dilution Sensors to measure access flow directly for an instant snapshot of access function. Transonic vascular access flow measurements detect flow limiting problems wherever they occur within a vascular access circuit: inflow, outflow and between the needles.
By measuring vascular access flow routinely and trending the results over several months, a record of access patency is created. A drop in access flow signals formation of a stenosis in time for proactive minimally invasive intervention.
Trending of vascular access flow over a one year time frame with PTA interventions is noted by arrows. Several technologies can monitor low AV access flow, but only fast-response blood-line reversal indicator dilution methods can trend flow. Their fast-response capability eliminates possible errors stemming from cardio-pulmonary recirculation.




